Navigating a chronic health condition or recovering from a significant illness often means embarking on a path of ongoing treatment. While these therapies are designed to improve your quality of life, understanding the full spectrum of Risks, Side Effects, & Long-Term Considerations is paramount. It's not just about today's dose; it's about how treatment weaves into the tapestry of your life, months and even years down the road. This guide empowers you to become an informed partner in your own healthcare journey, ensuring you approach ongoing treatments with clarity and confidence.
At a Glance: Your Roadmap to Understanding Ongoing Treatment Effects
- Ongoing treatments aren't just for acute problems: They manage chronic conditions (diabetes, hypertension) or extend well beyond initial recovery (cancer survivorship).
- Side effects aren't always immediate: Some manifest months or years after treatment concludes.
- Keep meticulous records: A summary of your treatment plan, dosages, and dates is crucial for future care.
- Your body systems are interconnected: Treatment for one area can affect your heart, bones, brain, or hormones.
- Communication is your most powerful tool: Talk openly with your healthcare team about all symptoms, concerns, and other medications.
- Lifestyle plays a major role: Diet, exercise, and stress management can significantly impact how you experience side effects.
- You're not alone: Mental health support is a vital component of long-term care.
- Know when to seek immediate help: Some severe symptoms require urgent medical attention.
The Long Haul: Why Ongoing Treatment Requires a Deeper Look
When a medication or therapy becomes a regular part of your life, whether daily for a chronic condition like diabetes or intermittently post-cancer, its impact extends far beyond its immediate effect. These ongoing treatments aim to control symptoms, prevent complications, and vastly improve your quality of life over the long term. But this sustained interaction between your body and treatment means continuous monitoring and a keen awareness of potential consequences are essential.
Think of it as tending a garden. You plant a seed (start a treatment) with good intentions, watering it regularly (taking your medication). You expect beautiful blooms (symptom control, improved health), but you also need to watch for pests (side effects) or changes in the soil (long-term impacts on your body) that might compromise its long-term health. It’s an active, ongoing process, not a one-time fix.
Decoding "Risks" and "Side Effects": What You Might Encounter
The terms "risks" and "side effects" are often used interchangeably, but it's helpful to consider side effects as typically anticipated, often manageable reactions, while risks refer to the broader potential for harm, including less common but more severe outcomes. Both are critical to understand when undergoing ongoing treatments.
Common Side Effects Across the Board
Many medications, regardless of their primary target, can cause a range of general side effects. These are the kinds of things your doctor might mention upfront, often manageable with dose adjustments or simple remedies:
- Gastrointestinal Issues: Nausea, upset stomach, diarrhea, or constipation are frequent companions to various medications.
- Drowsiness or Fatigue: Some treatments can make you feel sleepy or generally worn out. This is especially true for certain neurological or pain medications.
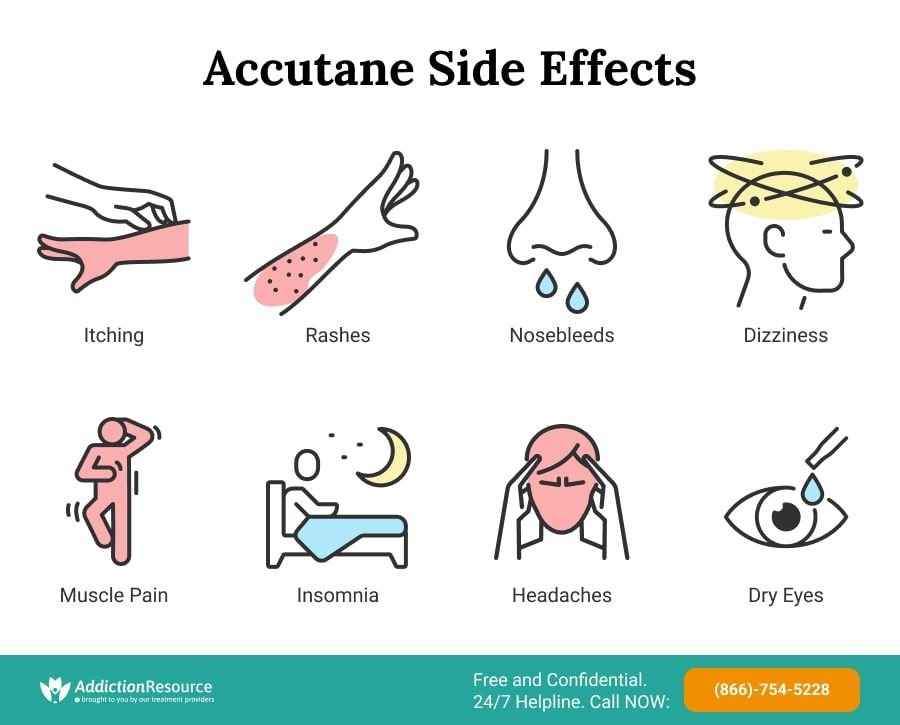
- Headache or Dizziness: A common reaction as your body adjusts to new compounds.
- Allergic Reactions: Rashes, itching, or hives can signal an allergy. While often mild, they warrant attention.
- Changes in Appetite or Weight: Medications can alter your metabolism or simply how appealing food seems, leading to weight gain or loss.
These effects can vary wildly from person to person. What's a minor inconvenience for one might be deeply disruptive for another. Always communicate how you’re feeling.
When "Side Effects" Become "Risks": Deeper Concerns
Beyond the common inconveniences, certain ongoing treatments carry more significant risks that necessitate close monitoring by your healthcare team. These aren't necessarily about immediate discomfort, but rather about the potential for long-term damage or severe adverse events.
For instance, medications might require periodic tests to monitor your:
- Liver or Kidney Function: These organs process and eliminate drugs, and prolonged use can sometimes strain them, necessitating blood tests to check their health.
- Blood Pressure: Some treatments can elevate blood pressure, increasing your risk for heart disease.
- Blood Counts: Certain therapies can affect your red or white blood cell counts, or platelets, impacting immunity or clotting ability.
In rare but critical instances, some symptoms demand immediate medical attention. These are the red flags you should never ignore: difficulty breathing, chest pain, signs of a severe allergic reaction (like swelling of the face or throat), or loss of consciousness. These aren't just side effects; they're potential life-threatening emergencies.
The Unique Landscape of Cancer Treatment Effects
Cancer treatments, while life-saving, are notoriously aggressive and can leave a lasting imprint on your body. Understanding these specific long-term and late effects is crucial for cancer survivors.
- Long-term (chronic) effects begin during treatment and persist afterward.
- Late effects emerge months or even years after treatment concludes, often catching people by surprise.
These effects aren't arbitrary; they're typically caused by a combination of factors including the specific type and dose of cancer treatment (e.g., chemotherapy, radiation, surgery, immunotherapy), the cancer itself, your age at diagnosis, your pre-treatment health, genetics, and even your lifestyle during and after treatment.
It’s critical to remember that not everyone experiences these effects, and their severity varies. But being aware empowers you to recognize them early and seek appropriate care. The cornerstone of managing these effects is maintaining a comprehensive record of your cancer treatment. Request a copy of your treatment plan or a summary detailing the types of treatments, doses, cycles, and any specific areas of your body that were treated. This document is a vital asset for your future healthcare teams, helping them diagnose new problems more effectively.
Navigating the Long-Term Terrain: Specific Conditions & Body Systems
Ongoing treatments, especially for chronic conditions or cancer, don't operate in a vacuum. They can affect various body systems, sometimes in subtle ways that only become apparent over time. Let's delve into some common areas of concern.
Hormonal and Metabolic Shifts
Your body's endocrine system, a network of glands that produce hormones, is exquisitely sensitive to external factors, including medications.
- Thyroid Troubles: Radiation to the head or neck, certain chemotherapies, or targeted therapies can disrupt your thyroid gland, leading to hypothyroidism (low thyroid hormones). Symptoms often include persistent fatigue, hair loss, dry skin, muscle cramps, anxiety or depression, and feeling perpetually cold. Regular thyroid level checks may become part of your routine.
- Sex Hormone Imbalances: Treatments affecting your ovaries or testes (surgery, radiation, hormone-blocking medicines, some chemotherapies) can lead to low estrogen in women and low testosterone in men. This can cause a cascade of symptoms: hot flashes, changes in memory and focus, bone loss, altered sex drive, and weight gain. Women may experience vaginal dryness and pain, while men might face erectile difficulties. Menstrual periods can become lighter, less frequent, or stop entirely.
Managing these shifts often involves hormone replacement therapy or other targeted interventions, always in consultation with an endocrinologist or your primary care provider.
Heart and Lung Health
The very treatments that save lives can, ironically, sometimes put stress on your vital organs.
- Cardiotoxicity (Heart Problems): Certain chemotherapies (like anthracyclines), immunotherapies, targeted therapies, some hormone therapies, and radiation to the chest can damage the heart muscle or its surrounding structures. This damage might manifest years later, leading to issues like heart failure, rhythm disturbances, or coronary artery disease. Your risk is higher if you smoke or have pre-existing conditions such as high blood pressure, high cholesterol, or diabetes. Regular cardiac screenings become essential for those at risk.
- Lung Problems: Chemotherapy drugs (like bleomycin or busulfan) or radiation to the chest can lead to lung damage, causing a persistent cough, shortness of breath, or wheezing. If these symptoms appear, a pulmonologist (lung specialist) consultation may be necessary to assess and manage the condition.
Neurological & Cognitive Impacts
Your brain and nervous system are intricate, and ongoing treatments can sometimes affect their function.
- Peripheral Neuropathy (PN): Chemotherapy, immunotherapy, targeted therapy, surgery, or even radiation can damage peripheral nerves, leading to numbness, tingling, or pain, most commonly in the hands and feet. This can range from a temporary nuisance to a permanent, debilitating condition, impacting balance and fine motor skills. Always report new or worsening nerve symptoms to your care team.
- Changes in Memory, Thinking, or Focus ("Chemo Brain"): Radiation to the brain or certain types of chemotherapy can cause subtle yet significant cognitive changes. You might find it harder to concentrate, recall words, multitask, or remember things. While often improving over time, these effects can be frustrating and impact daily life. Strategies like brain exercises, maintaining a routine, and discussing concerns with a neuro-psychologist can help.
Musculoskeletal and Connective Tissue Concerns
Bones, joints, and the tissues that support them are also susceptible to treatment effects.
- Bone, Joint, or Muscle Problems: Hormone-affecting treatments can contribute to osteoporosis (low bone density), increasing fracture risk. Chemotherapy, steroids, and certain hormone therapies can also cause generalized joint or muscle pain, especially if you're less active. Weight-bearing exercise, where appropriate, can help maintain bone density.
- Lymphedema: This is swelling caused by fluid buildup when lymph nodes are removed or damaged, often after surgery or radiation for cancers like breast or head/neck cancer. It can start years later and affect mobility, self-image, and increase the risk of infection. Early detection and management, often with specialized physical therapy and compression garments, can often reverse or significantly improve lymphedema.
Oral and Sensory Health
Your mouth, eyes, and ears are often overlooked, but their health can be impacted significantly.
- Teeth or Mouth Problems: Chemotherapy can damage tooth enamel, increasing cavity risk. Radiation to the head, neck, or brain can cause chronic dry mouth (xerostomia), which also boosts cavity and tooth loss risk, making regular dental visits (every 6 months) essential. A rare but serious condition called osteonecrosis of the jaw (ONJ), where jawbone cells die, can result from radiation to the jaw or certain bone-strengthening medications (bisphosphonates). Dental evaluation before treatment and rigorous oral hygiene are crucial.
- Hearing Loss: High-dose chemotherapy (especially platinum-based drugs), radiation to the head, ear, or brain, and certain antibiotics can cause permanent hearing loss. Hearing aids or a referral to an ENT specialist or audiologist may be beneficial.
- Vision Changes: Radiation to the head or eye, certain chemotherapy drugs, targeted therapies, immunotherapies, and hormone therapies can cause various vision problems, including cataracts, glaucoma, dry eyes, redness, or irritation. An ophthalmologist consultation may be needed for diagnosis and management. Find out if LASIK is worth it if you're considering vision correction options, as your long-term treatment history could influence suitability.
Bowel, Bladder, and Digestive Wellness
The digestive and urinary systems are frequently impacted by ongoing treatments.
- Gastrointestinal Issues: Beyond the acute nausea and upset stomach, long-term medication use can sometimes lead to chronic issues like irritable bowel syndrome (IBS)-like symptoms, malabsorption, or persistent changes in bowel habits.
- Bowel or Bladder Problems: Surgery or radiation to the abdomen or pelvis can cause a range of issues, from bowel blockage or chronic diarrhea to urinary retention or incontinence. Bladder and urinary tract infections can also become more frequent. These issues can profoundly affect daily comfort and quality of life, requiring specialized medical or rehabilitative approaches.
Beyond the Physical: Mental & Social Wellbeing
The effects of ongoing treatments aren't limited to physical symptoms. The emotional, psychological, and social toll can be just as significant, if not more so.
- Mental Health and Distress: Many individuals undergoing or recovering from long-term treatments experience significant mental health challenges. This can include anxiety, depression, post-traumatic stress disorder (PTSD), chronic loneliness, and a pervasive fear of recurrence (especially for cancer survivors). Feelings of resentment, survivor's guilt, concerns about discrimination, and worries about relationships are also common. Recognizing these feelings is the first step; seeking support from family, friends, and mental health professionals (therapists, counselors, psychiatrists) is a vital component of holistic care.
- Sexuality and Fertility Problems: Treatments affecting the reproductive system (certain chemotherapies, radiation to the pelvis or belly) can cause temporary or permanent fertility issues. Discussing fertility preservation options before treatment is critical if having biological children is important to you. Beyond fertility, ongoing treatments can also impact sexual organs, reduce sex drive, impair sexual function, and negatively affect body image and overall well-being. These are sensitive topics, but your cancer care team or primary care provider can often refer you to specialists who can offer support and solutions.
Proactive Management: Your Role in Minimizing Risks
While healthcare providers are your expert guides, you are the central figure in your own care. Taking a proactive stance can significantly minimize risks and enhance your overall well-being.
Open Communication with Your Care Team
This is perhaps the most crucial element. Your healthcare providers can only help you effectively if they have a complete picture.
- Share Everything: Always provide a full list of all medications you're taking, including over-the-counter drugs, supplements, and herbal remedies. Inform them about any known allergies, your complete medical history, and lifestyle factors like alcohol use, smoking, or dietary habits.
- Ask Incisive Questions: Don't hesitate to ask your healthcare team:
- "What are the possible long-term and late effects of my treatment(s)?"
- "Do I have a higher risk for certain effects based on my health history?"
- "Is there anything I can do proactively to prevent or manage these effects?"
- "Could these treatments affect my fertility or increase my risk for second cancers?"
- "Which cancer screening tests should I get and how often, especially given my treatment history?"
- "What other specialists (e.g., cardiologist, endocrinologist, physical therapist, mental health professional) or follow-up care should I anticipate?"
- "Could cancer rehabilitation help me?"
- "When should I contact my primary healthcare team versus my specialist care team for new symptoms?"
Adherence and Monitoring
Sticking to your treatment plan and attending follow-up appointments are non-negotiable for safety and effectiveness.
- Take Medication as Directed: Deviating from dosage or schedule can reduce effectiveness or increase side effects. If you're struggling with adherence, discuss it openly with your doctor, don't just stop taking it.
- Regular Follow-Ups and Tests: Attend all scheduled appointments. These visits are vital for your healthcare team to assess treatment effectiveness, monitor for side effects, adjust dosages if necessary, and order periodic tests like blood work, liver/kidney function tests, or imaging scans.
- Know When to Consult: For new or worsening symptoms, side effects that interfere with daily activities, questions about your medication, considering other substances, or needing clarification on administration or storage, consult your clinician.
- Immediate Medical Attention: For severe, sudden symptoms like difficulty breathing, chest pain, signs of a severe allergic reaction (e.g., swelling of the face or throat), or loss of consciousness, seek immediate emergency medical attention.
Understanding Interactions
Medications are powerful, and their effects can be altered by other substances.
- Drug-Drug Interactions: One medication can affect how another is absorbed, metabolized, or eliminated, leading to reduced effectiveness or increased side effects. This is why a complete medication list is so important.
- Drug-Supplement/Herbal Interactions: Many "natural" products can interact with prescription medications. Always disclose all supplements to your doctor and pharmacist.
- Drug-Food Interactions: Certain foods (e.g., grapefruit juice with statins) or even alcohol can interact with medications, so always ask about dietary restrictions.
Lifestyle as a Treatment Partner
Your daily choices play a significant role in how your body handles ongoing treatments.
- Nutrition: A balanced, healthy diet can support your immune system, energy levels, and overall recovery.
- Physical Activity: Where appropriate and approved by your doctor, regular exercise can combat fatigue, improve mood, strengthen bones, and maintain muscle mass.
- Stress Management: Techniques like mindfulness, meditation, or gentle yoga can help manage anxiety and improve sleep quality.
- Avoid Smoking and Excessive Alcohol: These can exacerbate certain side effects, interfere with treatment effectiveness, and increase the risk of other health problems.
Documentation is Power
As mentioned, keeping a record of your medical history, especially treatment specifics, is invaluable. For cancer survivors, a detailed cancer treatment summary is a non-negotiable document that should be shared with all future healthcare providers. It helps them understand your unique vulnerabilities and potential long-term effects.
Special Considerations: Who Needs Extra Vigilance?
While everyone on ongoing treatments should be vigilant, certain groups require particular attention due to increased sensitivity or unique risk factors.
- Older Adults: As we age, our bodies metabolize drugs differently, and we may be more sensitive to side effects. Older adults also often take multiple medications, increasing the risk of interactions.
- Individuals with Chronic Health Conditions: Those with pre-existing heart disease, diabetes, respiratory issues, or other chronic conditions may be more vulnerable to certain treatment-related complications.
- Pregnancy or Breastfeeding: Many medications can pose risks to a developing fetus or be passed through breast milk. Treatment decisions in these circumstances require careful discussion with healthcare providers to weigh risks versus benefits.
- Individuals with a History of Substance Use or Mental Health Disorders: These conditions can complicate treatment adherence, increase sensitivity to certain medications, or interact negatively with therapies. Open communication with your care team is vital.
- Known Allergies or Hypersensitivity: A history of allergic reactions to medications or other substances is a critical piece of information that must always be shared with your healthcare team to prevent severe adverse reactions.
- Severe Liver or Kidney Impairment: Since these organs are crucial for drug metabolism and elimination, their impairment significantly alters how medications are processed, often requiring dose adjustments or avoidance of certain drugs.
The Future of Your Health: Screenings and Second Cancers
One of the most sobering long-term considerations, particularly for cancer survivors, is the increased risk of developing a new, secondary cancer—distinct from a recurrence of the original disease. Certain cancer treatments, such as radiation and specific chemotherapies, can sometimes induce these secondary malignancies years or decades later.
This underscores the importance of a lifelong partnership with your healthcare team. You should proactively discuss:
- Individual Risk: Understand your specific risk profile for secondary cancers based on your past treatments and personal health history.
- Lifestyle Factors: Discuss how your lifestyle choices (e.g., diet, exercise, smoking cessation) can influence your risk.
- Family History: Update your care team on any new family cancer diagnoses.
- Recommended Screenings: Confirm which routine cancer screenings (e.g., mammograms, colonoscopies, skin checks) are recommended for you, and at what frequency, especially in light of your treatment history. For example, if you received chest radiation, you might require earlier or more frequent breast cancer screenings.
Regular follow-up appointments are not just about managing existing effects; they're also about proactive surveillance for potential new health challenges.
Empowering Your Journey: Take Control of Your Health Story
Embarking on a journey with ongoing treatments requires more than just passively taking medication; it demands active participation, keen observation, and unwavering communication. The Risks, Side Effects, & Long-Term Considerations are not meant to frighten you, but to equip you with the knowledge needed to advocate for your best health.
By understanding what to expect, by meticulously documenting your treatment history, and by fostering an open, honest dialogue with your entire healthcare team, you transform from a patient into an empowered partner. You are the expert on your own body and how treatments affect it. Your voice is crucial. Remember, your health story is continuously being written, and with vigilance and knowledge, you can help guide it towards the best possible outcome.